Should you get a stent
Mr Lim was lying on the table during an angiogram procedure and I had just finished explaining the coronary angiogram pictures showing a 99 per cent blockage of his right coronary artery (RCA). What Mr Lim was asking me was the type of stent I was going to put into his blocked artery.
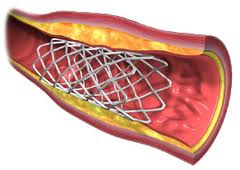
Stents are small mesh-like tubular metal structures used as a scaffolding to keep an artery open after balloon angioplasty. It helps to prevent about 30 per cent of arteries which will otherwise become blocked again after a simple balloon inflation.
Broadly speaking, there are two kinds of coronary stents – the bare metal stents (BMS) and the drug-eluting stents (DES). Reader MAB wrote recently asking about coronary stents and in the Heart2Heart issue on Aug 25, I explained what a stent is and how it works but was not able to expand on the topic due to space constraint.
Angioplasty and stent insertion causes injury to the wall of the artery. As the artery heals, endothelial tissue grows around the stent holding it in place. This makes it very unlikely for a stent to move after it has been placed in an artery.
In some cases, there is an overgrowth of this scar tissue that lines the stent and if the growth is unchecked, it can lead to narrowing of the artery. This happens in about 20 per cent of cases, and we are back to square one!
To overcome this problem, this scar tissue overgrowth has to be suppressed. It is a bit like trying to stop the growth of cancer cells. In fact, the 1990′s saw extensive research looking into the use of anti-cancer drugs to prevent tissue overgrowth and consequent re-narrowing (restenosis) of the artery.
This led to the birth of the first drug-coated stent, generally known as DES, using the drug Sirolimus in 2002.
The use of DES became very popular almost instantly. Re-narrowing of arteries which was the bane of interventional cardiologists suddenly had a remedy.
The reduced risk of re-narrowed arteries – down to 5 to 10 per cent – meant less need for repeat hospital admissions for angioplasty procedures and also prevented the need for open-heart coronary artery bypass surgery.
More and more complex cases are now able to be done, such as arteries with long blockage, smaller sized arteries, fresh (acute) heart attack and totally (100 per cent) blocked arteries with good results. DES have indeed revolutionised the way coronary heart disease is treated in the new millennium.
However, it was not long before we realised that DES had their problems too. There was an increase in the incidence of blood clot forming within the DES called stent thrombosis (ST). Whilst restenosis from BMS causes symptoms of stable angina (chest pain during activity), ST can cause sudden blockage of the artery leading to heart attack with possible dire consequences.
The BASKET-LATE trial which compared the incidence of ST between BMD and DES was published in late 2006. It showed that DES had incidence of ST 2 to 3 times higher, and heart attack risk about four times greater.
The results of this study were soon made known to the world. This struck a chord of fear and uncertainty in the hearts of not just the public, but also everyone involved in the care of heart patients.
When the ST cases were examined, it was found that the incidence of ST was higher in those cases where the blood-thinning drug, clopidogrel, was stopped somewhat prematurely. Clopidogrel is similar to aspirin in that it opposes the action of platelets but the two have to be given in combination to get maximum effect.
So what has become of DES after all that?
The use of DES did take a knock after the release of the BASKET-LATE results but recovered soon after when the medical world understood the process of ST better and how to avoid it. If anyone were to have an angioplasty with an insertion of a DES or two, the following statements may help:
- Take aspirin indefinitely, unless told otherwise by your doctor or cardiologist.
- Take clopidogrel for at least a year. It may even be longer in certain cases such as multiple DES insertion, restenosis of a DES and those who are known to have increased likelihood of blood clot forming in the circulatory system. If clopidogrel (or aspirin) needs to be stopped for any reason such as before a surgery, please consult your cardiologist. It can be very dangerous to stop clopidogrel or aspirin prematurely.
- Take all the other heart medications as your doctor has prescribed. These drugs work well together.
In general, DES are used mainly in long artery blockages, relatively small-sized arteries, diabetic patients and the artery supplying the front aspect of the heart (the left-anterior descending artery), amongst other indications.
So for Mr Lim, with his RCA at 3.5mm in size and a blockage of about 10mm in length – that is a short blockage in a big-sized artery – my reply would be, “A bare metal stent is just fine, Mr Lim.”

No comments:
Post a Comment